A Word on Pill Shaming
There are a number of reasons that prevent people from seeking, and ultimately receiving mental healthcare. Clearly, structural barriers contribute to these cases (i.e. some tangible lack of access to medicine). More subtle but no less pervasive, is the societal role in creating the taboo surrounding mental illness. Among people in the US reporting an unmet mental health need, over 40% reported that some attitudinal barrier contributed to them not receiving treatment[17]. These barriers are direct functions of our perception of mental illness, and subsequently receiving medicinal treatment. Pill shaming is a commonly experienced phenomenon among those seeking out or utilizing medicinal resources for mental illness, in which someone expresses negative opinions or disdain in response to hearing that another person is using medication to treat a mental health issue[14]. It seems very likely that this contributes to the common responses of, “I can work it out on my own,” or “I’m not crazy, I don’t need pills to confront my problems,” when a person is asked why they did not receive treatment. Furthermore, it also contributes to one of the primary difficulties of treating mental illness—getting patients to follow their treatment plan.
The phenomenon of pill shaming contrasts sharply with the medical culture surrounding diabetes, for example, whose sufferers might be ridiculed for refusing to take insulin. This particular societal pressure is referred to as the sick role—a social construct of how society believes a sick person should conduct themselves, containing certain rights allotted to those suffering from a medical ailment, but also certain responsibilities placed on those people. Among these rights are the exemption from typical social duties (i.e. work, school), and the assumption that the sufferer is not responsible for their illness. Among the responsibilities are that the sufferer actively try to improve, and that they seek and submit to appropriate medical treatment (i.e. a person with diabetes is expected to see all the doctors, and undergo all treatment necessary to manage their condition)[12]. Pill shaming as a practice is in direct conflict with the way we as a society have decided medical conditions should be addressed.
The conversation around mental illness needs to be continued. If those suffering felt empowered seeking out mental health resources, as opposed to ashamed, we would experience much improved mental health outcomes. These treatments work. Though antidepressants are often continued for roughly a year to 18 months after improvement is noticed (to minimize possibility of symptoms returning), up to 60% of patients report significant relief of their symptoms in their first 6-8 weeks[9].
Because depression arises from a variety of mechanisms and causes, the best treatment plan differs between patients [4]. Medical treatment of depression is all about finding the medication that suits your symptoms and presentation of depression most appropriately. Put another way, the medication that suits a specific case of depression the best, is the one that deals most directly with the mechanism of that case (i.e. a chemical imbalance, incomplete pathway, etc.). A few of the mechanisms most targeted by antidepressant medication will be discussed below.
Antidepressants
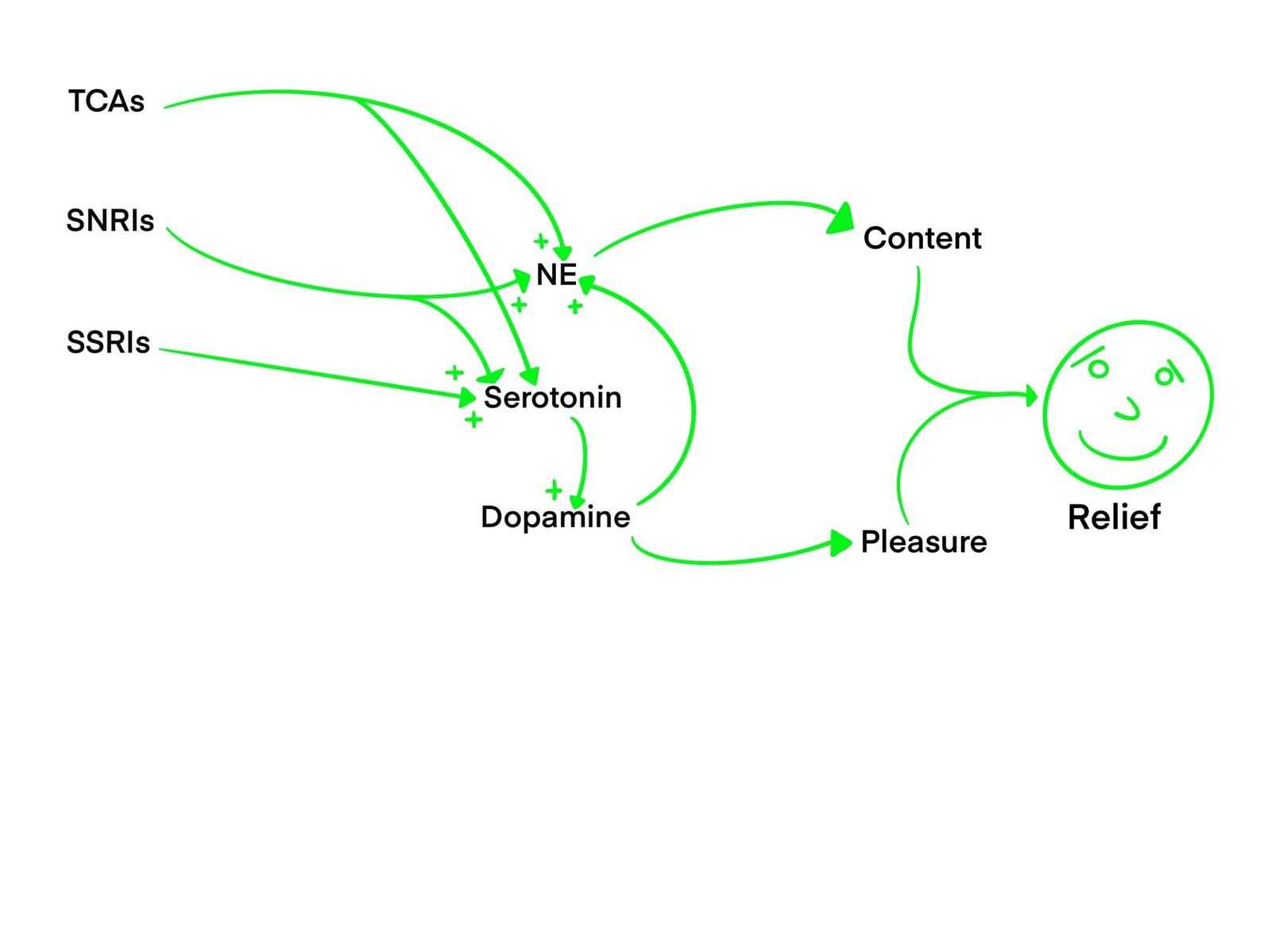
What nearly all antidepressants have in common is that they work by controlling the amounts of 3 key neurotransmitters in the brain: serotonin, norepinephrine, and dopamine. Serotonin is an agonist of cells that release dopamine—an essential neurotransmitter in the Reward Network that makes one feel happy[16][3]. High levels of dopamine also lead to the release of norepinephrine [8]. Norepinephrine, often abbreviated as NE, is an agonist of neurons that promote wakefulness and cognition, which may lead to people feeling more alert, capable, and confident[3]. Antidepressants are used to increase the amount of these chemicals that the brain releases. The reason for this approach is based upon the theory that depressed people naturally have low levels of these chemicals in their brain. As such, different classes of antidepressants have been developed to achieve typical levels of these chemicals by affecting the cells responsible for their release, and thus alleviate depressive symptoms.
Some Useful Terminology
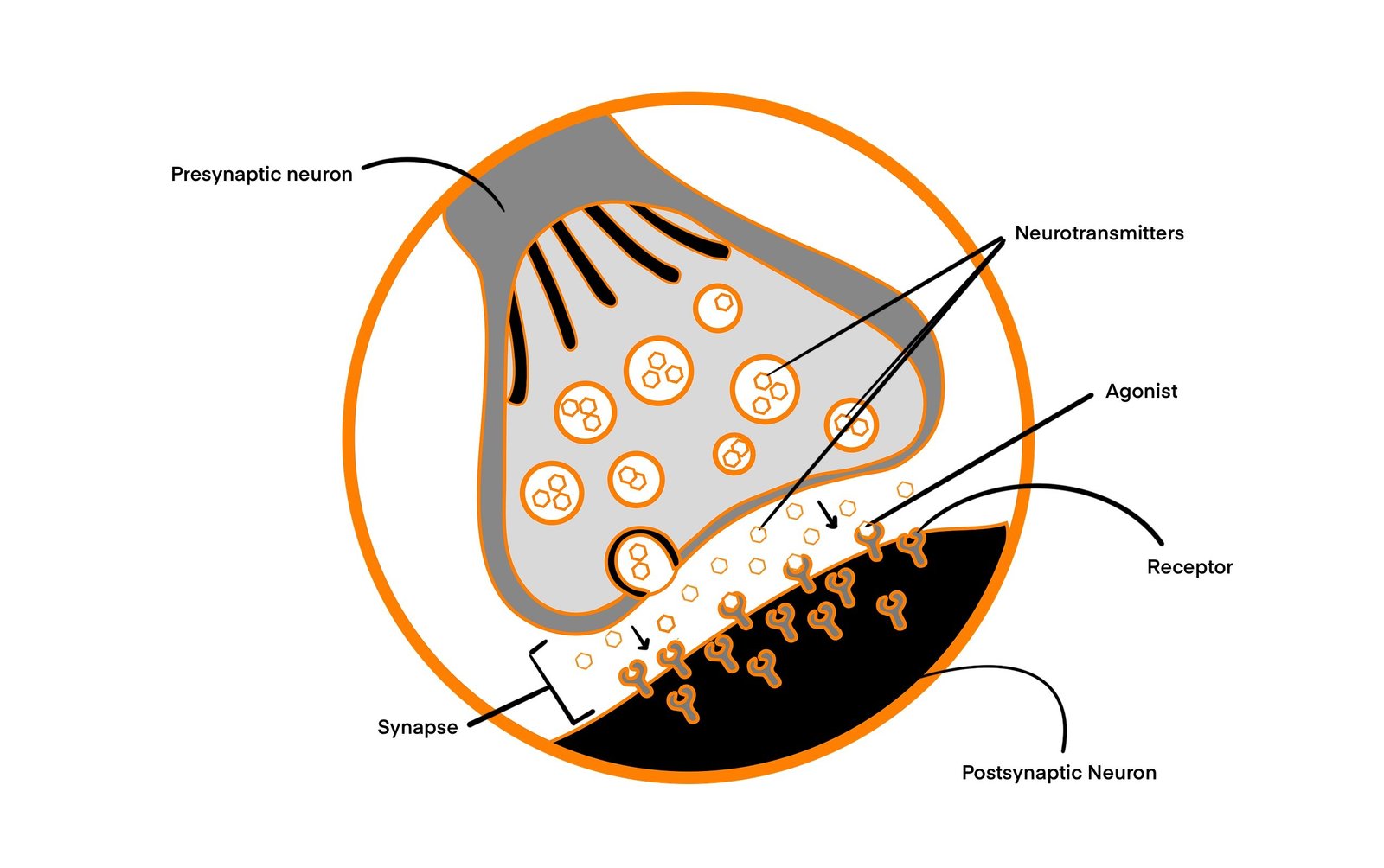
At the most basic level, communication in the brain is controlled by the release and sensation of chemicals at a synapse (the gap between two communicating brain cells, or neurons). The cell sending the signal is referred to as the presynaptic neuron, and the cell that receives the signal is referred to as the postsynaptic neuron. Neurotransmitters are the chemicals that brain cells use to communicate with each other, and are stored in compartments called vesicles.

Neurotransmitters are the chemical signals that are released into the synapse by the presynaptic neuron, to be sensed and acted upon by the postsynaptic neuron. When a neurotransmitter is released in the brain, it attaches to a specific receptor. The common name for an agent such as a neurotransmitter that binds a receptor, is called a ligand. A ligand that activates the receptor (and similar chemicals that activate the same receptor), are referred to as agonists, and those that block or inhibit the receptor are referred to as antagonists. Both of these types of chemicals compete to “fit” into the shape of the receptor. The key difference is that agonists activate the postsynaptic cell, while antagonists block the receptor so no agonists can bind

The activation of a receptor regulates activity of the postsynaptic neuron, either activating it to send its own signal, or inhibiting it from doing so. Afterwards, the agonist unbinds from the receptor, and can be taken back up into the presynaptic cell in new vesicles. This process takes place around 100 billion times per second and is the fundamental means of information flow in the brain [18].
Common Antidepressants
SSRIs (Selective Serotonin Reuptake Inhibitors) are antidepressants that prevent the recycling step of the process in which serotonin would typically be reabsorbed by the presynaptic neuron. The result—an increase of serotonin in the synapse—allows for serotonin to be more readily available to activate receptors on the postsynaptic neuron. This leads to an increase in dopamine release in regions of the brain’s reward network (RN) [15]. A lack of dopamine is thought to cause the feeling of numbness, or lack of pleasure in depressed patients [1]. As such, the aim of SSRIs is to address this deficit by increasing the amount of serotonin in the brain, thereby increasing the amount of dopamine released into the RN.
SNRIs (Serotonin Norepinephrine Reuptake Inhibitors), perhaps unsurprisingly, work in a similar way to SSRI’s, except in that these drugs prevent the reuptake of serotonin and norepinephrine. Norepinephrine, unlike serotonin, is not known to directly agonize the release of dopamine in the reward network[3]. Rather, norepinephrine’s effects on depression likely lie in their ability to enhance what is known as executive function, supported by a Cognitive Control Network (CCN). This ability is heavily implicated in the way we address conflict, both social and cognitive [3][2]. Notably, it helps us to control our emotions in light of conflict. Executive function also supports the ability to resist urges and impulses, which may help patients taking SNRIs avoid reverting to unhealthy coping mechanisms. Though there has been debate between which medication is more effective, research shows that SSRIs and SNRIs are roughly equally helpful for patients, on average[11].
TCAs (Tricyclic Antidepressants) are members of the first generation of antidepressants. They are typically prescribed after other antidepressants such as SSRIs. The reason for this is that TCAs are a bit more aggressive as a treatment option when compared to other antidepressants, and thus lead to more side effects[13]. Like SNRIs, TCAs prevent the reuptake of serotonin and norepinephrine. Unlike the other drugs listed here however, TCAs are less selective with regard to where they bind, and as such inhibit the release of at least three other neurotransmitters, acting as an antagonist. One such example is acetylcholine, which plays a role in anxiety and ADHD, in addition to depression [8]. For this reason, TCAs are often not the preferred treatment for someone suffering exclusively from depression, but can be very useful for people with resistant depression or who experience more dynamic symptoms of mental illness.
Future Antidepressants
It was found in research from 2016 that SSRIs work by a second, longer-acting mechanism, which explains why these drugs can take 4-6 weeks to take full effect[6]. While this time period is not ideal, some relief can begin to be felt within 1-2 weeks [9]. Current research into this second mechanism will likely allow for the shortening of the interim period, as well as the development of more personalized medical treatments for depression in the future [6].
Takeaways
Depression is a very prevalent problem that affects people of all ages and backgrounds. This article delves into just a few of many treatments that have been effective in addressing depression. Everyone’s healing looks different, so one should not be discouraged, should one method or another not help them. Medication, behavioral changes, and therapies, as well as the use of novel technologies all show promising results in helping people manage the effects of depression in their lives. Improvement can, and does happen when people receive proper treatment. The picture of how that treatment looks depends entirely on the individual. Often, a combination of approaches is very helpful for people, such as medication in conjunction with a therapeutic approach.
Furthermore, these methods are only getting more effective. Research is constantly being conducted, new medications synthesized, new technologies designed. By the time an individual could conceivably exhaust their options in the realm of addressing depression, there would be several new avenues for them to explore—and that is only including methods that have been shown to be effective. New components are implicated in depression as more research is done, and thus new methods of approach are discovered. The vast array of potent treatments for depression is only growing, and as such people who suffer from depression should be encouraged to seek treatment.
~ Gabe Sweezy

Gabe Sweezy is an undergraduate student of neuroscience and a premedical student at Saint Louis University. As a student of cognitive neuroscience with a passion for mental health, Gabe is particularly interested in the biological processes underlying mental illnesses.
This research article is supervised and sponsored by Faculty Sponsor, Dr. Brenda Kirchhoff Ph.D.
References
[1] Belujon, P., & Grace, A. A. (2017). Dopamine System Dysregulation in Major Depressive
Disorders. International Journal of Neuropsychopharmacology, 20(12), 1036–1046.
https://doi.org/10.1093/ijnp/pyx056
[2] Briley, M. (2010). Improvement of social adaptation in depression with serotonin and
norepinephrine reuptake inhibitors. Neuropsychiatric Disease and Treatment, 647.
https://doi.org/10.2147/ndt.s13171
[3] Briley, M., & Chantal, M. (2011). The importance of norepinephrine in depression.
Neuropsychiatric Disease and Treatment, 7, 9. https://doi.org/10.2147/ndt.s19619
[4] Cipriani, Andrea, Toshi A Furukawa, Georgia Salanti, Anna Chaimani, Lauren Z Atkinson, Yusuke
Ogawa, Stefan Leucht, et al. 2018. “Comparative Efficacy and Acceptability of 21 Antidepressant Drugs
for the Acute Treatment of Adults with Major Depressive Disorder: A Systematic Review and Network
Meta-Analysis.” The Lancet 391 (10128): 1357–66. https://doi.org/10.1016/s0140-6736(17)32802-7.
[5] Chm.bris.ac.uk. 2022. The method of synaptic transmission is outlined below. [online] Available at:
<http://www.chm.bris.ac.uk/webprojects2006/Cowlishaw/mech%20synaptic%20transmission.htm>
[6] Erb, S. J., Schappi, J. M., & Rasenick, M. M. (2016). Antidepressants Accumulate in Lipid
Rafts Independent of Monoamine Transporters to Modulate Redistribution of the G Protein, Gαs.
Journal of Biological Chemistry, 291(38), 19725–19733.
https://doi.org/10.1074/jbc.m116.727263
[7] FIG. 1. Pathways for synthesis of dopamine, noradrenaline, adrenaline,… (n.d.).
ResearchGate. Retrieved March 5, 2022, from
https://www.researchgate.net/figure/Pathways-for-synthesis-of-dopamine-noradrenaline-adrenali
ne-and-serotonin-5-HTP_fig1_47675740
[8] Higley, M. J., & Picciotto, M. R. (2014). Neuromodulation by acetylcholine: examples from
schizophrenia and depression. Current Opinion in Neurobiology, 29, 88–95.
https://doi.org/10.1016/j.conb.2014.06.004
[9] Information, N. C. for B., Pike, U. S. N. L. of M. 8600 R., MD, B., & Usa, 20894. (2020).
Depression: How effective are antidepressants? In www.ncbi.nlm.nih.gov. Institute for Quality
and Efficiency in Health Care (IQWiG).
https://www.ncbi.nlm.nih.gov/books/NBK361016/#:~:text=In%20other%20words%2C%20antid
epressants%20are
[10] Khan Academy. 2022. Ligands & receptors (article) | Khan Academy. [online] Available at:
<https://www.khanacademy.org/science/ap-biology/cell-communication-and-cell-cycle/signal-
transduction/a/signal-perception>
[11] Machado, M., & Einarson, T. R. (2009). Comparison of SSRIs and SNRIs in major
depressive disorder: a meta-analysis of head-to-head randomized clinical trials. Journal of
Clinical Pharmacy and Therapeutics, 35(2), 177–188.
https://doi.org/10.1111/j.1365-2710.2009.01050.x
[12] Mitchell, E. and Mitchell, E., 2022. NHS England » The sick role. [online] England.nhs.uk.
Available at: <https://www.england.nhs.uk/blog/ed-mitchell-2/> [Accessed 14 March 2022].
[13] Moraczewski, J., & Aedma, K. K. (2020, December 7). Tricyclic Antidepressants. PubMed;
StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557791/
[14] Namiillinois.org. 2022. How ‘Pill Shaming’ Hurts Those Who Take Medications for Mental Health
–NAMI Illinois. [online] Available at: <https://namiillinois.org/how-pill-shaming-hurts-those-who-take-
medications-for-mental
health/#:~:text=Pill%20shaming%20occurs%20when%20someone,to%20work%20through%20tough%
20times.> [Accessed 14 March 2022].
[15] Nautiyal, K. M., & Hen, R. (2017). Serotonin receptors in depression: from A to B.
F1000Research, 6, 123. https://doi.org/10.12688/f1000research.9736.1
[16] Neuroanatomy and Physiology of Brain Reward II. (2020). Colorado.edu.
http://ibg.colorado.edu/cadd1/a_drug/essays/essay4.htm
[17] Rowan, Kathleen, Donna D. McAlpine, and Lynn A. Blewett. 2013. “Access and Cost Barriers to
Mental Health Care, by Insurance Status, 1999–2010.” Health Affairs 32 (10): 1723–30.
https://doi.org/10.1377/hlthaff.2013.0133.
[18] Signal propagation: The movement of signals between neurons (article) | Khan Academy.
(2019). Khan Academy; Khan Academy.
https://www.khanacademy.org/test-prep/mcat/organ-systems/neural-synapses/a/signal-propagatio
n-the-movement-of-signals-between-neurons