What is Depression?
One of the world’s leading causes of disability, depression is a mental illness that is frequently experienced with symptoms of dejected moods, disinterest, excessive self-criticism, and many others. Given the pervasiveness of depression as an illness, you might think people would readily discuss it. There are a lot of reasons why this is not the case—the stigmatization of mental illness and seeking help being at the forefront. People with mental illness are often mischaracterized as weak, or as damaged. Depression, however, is fundamentally an issue of health. A depressed person has a medical illness. Is a person with a broken arm weak? Or is it because they are weak that they broke an arm? Of course not. So, where is the disconnect that keeps people from understanding depression the same way they might understand a broken bone? A large contributor is ignorance.
Frankly, that is understandable. Depression is hardly understood comprehensively as a disease. To make matters worse, there is such variance in the experience of depression, that a definitive diagnosis based on symptoms is difficult to confer[7]. There is no x-ray machine you can go through and demonstrate your depression—no peculiar white swab to put up your nose and poke your brain with either. But, modern neuroscientific research imaging techniques, as well as studies done on depressed patients have shed some light on from where depression might arise. My hope is that with a better understanding of depression as a disease—and not as a spectral boogeyman—that depression starts to be addressed more appropriately and comprehensively. There are great treatment options for mild to severe depression, as will be discussed at length in a later article.
Where is Depression?
This model of depression lends a few key insights into the nature of the disorder. Primarily, the experience of depression is additive—the expression of one’s symptoms are proportional to the disfunction of at least four different networks. The degree to which each connection is enhanced or impeded is also variable. This may lend some explanation to the lack of uniformity in depression’s symptoms. Additionally, as will likely be the subject of future research[6], there are likely integrative symptoms of depression that are affected by the interactions between these networks. This makes sense with our model; if you look at the diagram above, you can see many overlaps between flows of information through the same regions. Lastly and perhaps most obviously, there are a lot of factors at play with regards to the prevalence of depression in the brain—not only does there exist a mechanistic explanation of depression, but one that is quite elaborative.
Some earlier research attempted to pin down depression on one cause or another—one molecular interaction or one region of the brain. And while this research, yes, contributes to the scientific understanding of depression, more recent evidence describes a much larger picture of depression: one explained by atypical connections between many brain networks. A brain network is a group of brain regions (or parts of your brain), that act together to accomplish certain cognitive tasks or processes. The implication of irregular connections in multiple networks in depressed patients can help us to identify specific components of the disease. To our knowledge, there are at least four functional brain networks involved in the experience of depression[6]. In two of these networks, the connections are on average, stronger in depressed patients; in the other two networks, the connections are on average, weaker in depressed patients. Below is a visual representation of a modern, network-centered view of depression.

Atypical patterns of connectivity in neural networks of depressed patients
This explains why depression has historically been so difficult to understand from a scientific perspective. Nonetheless, this is the 21st century, and modern neuroscience imaging and research techniques have revealed a lot about depression in the last couple decades. Below is a breakdown of the networks that have been implicated in depression through scientific research, and how they affect the depressed individual.
Why (and where) You Feel Sad
Principally, depressed individuals report the experience of intense sadness. The Affective Network (AN, pictured above in yellow) is responsible for emotional regulation and processing in your brain. You experience an event, and the AN tells you how to feel about that event. A few key players in this include the amygdala, the hippocampus, and the anterior cingulate cortex. The hippocampus is also associated heavily with the memory of events and experiences, which may help explain why people with traumatic memories are at higher risk for depression.
The hippocampus (HIP), amygdala (AMY), and anterior cingulate cortex (ACC) of the Affective Network and Limbic System
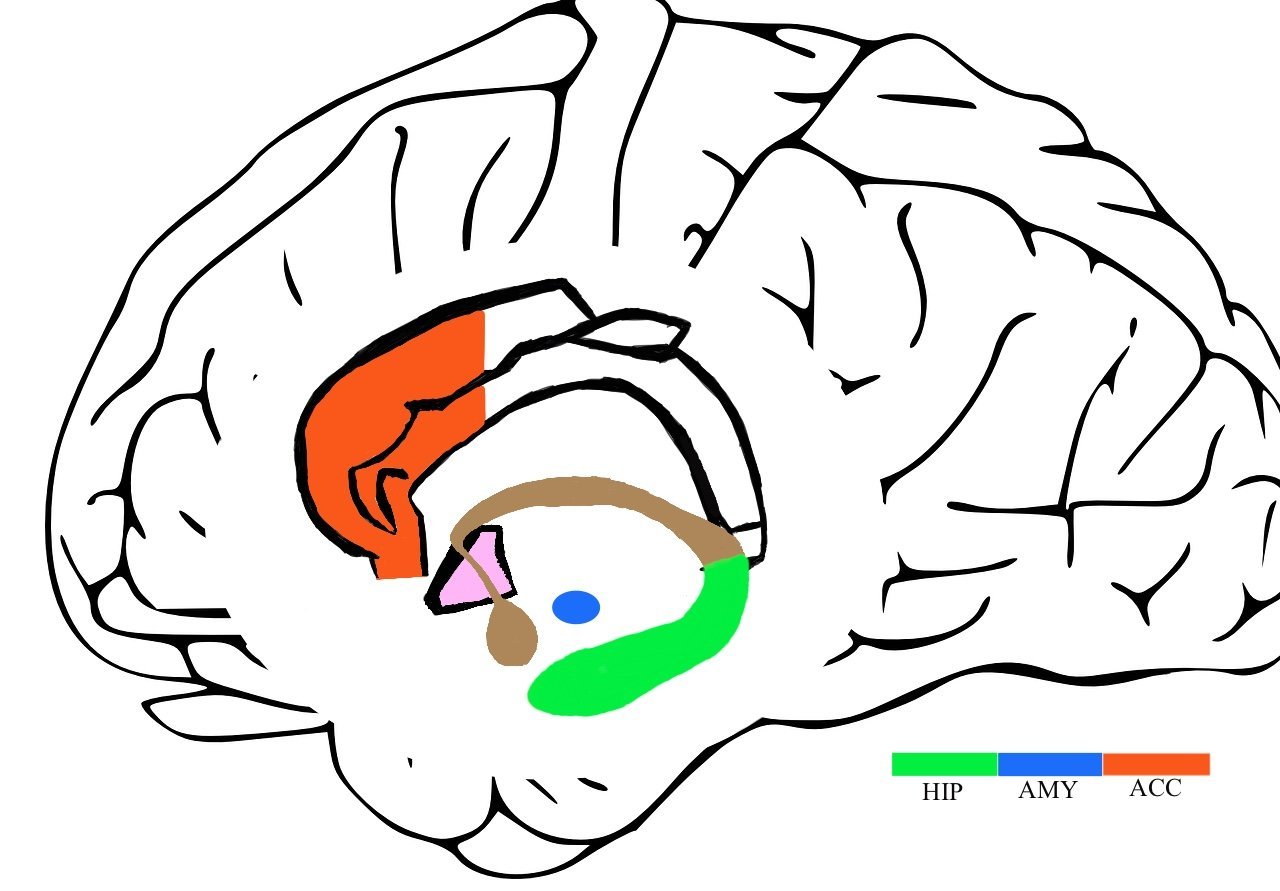
The hippocampus (HIP), amygdala (AMY), and anterior cingulate cortex (ACC) of the Affective Network and Limbic System
In depressed patients however, the connections in this network are stronger than average[2]. The signal associated with a certain feeling of sadness, is relayed in much greater numbers than appropriate. So, the emotional attribution placed on events that might normally feel like an inconvenience, might make your brain feel like you’ve undergone a tragedy. The cells responsible for telling you how to feel are physically more sensitive: more connections mean more sensors.
Why You don’t Feel Happy
You may be thinking, if the AN is more sensitive, does that mean that happy things should feel happier? And while many people who experience depression also do have episodes of euphoria, this is not the case for many depressed individuals on account of another network.
The Reward Network (RN, pictured above in blue) responds to positive events by releasing chemicals that make you feel good. This is from where the sensation of pleasure arises. Imaging studies (fMRI, EEG, etc.) of depressed patients, however, show that the connections in the Reward Network are on average, weaker[1]. This has been theorized to explain the symptom of anhedonia (lack of pleasure) in depressed patients.
Why You keep Feeling Sad
Even when you aren’t trying to think about anything, your brain won’t let that slide. The Default Mode Network (DMN, pictured above in red) is the network in your brain that is most active when you’re mind wandering. The DMN has been theorized, amongst many other things, to be responsible for thoughts of the self and of the future. As you may have guessed by this point, depressed patients on average, show enhanced connection of the regions in the Default Mode Network[5]. This has been theorized to be responsible for rumination, or the tendency to become fixated on depressive thoughts. It may play an especially important role in depressed patients with particularly inappropriate or incongruent ideas of themselves. This is consistent with the reports of many depressed patients, as many describe these feelings as persistent. This also lends some support to the idea that the length of time for which a person experiences depressive symptoms is indicative of its presence and severity (used for clinical diagnoses).
You may ask—why can’t you think of something else? Would directing your attention elsewhere help prevent mind wandering? The healthy non-depressed patient (and likely some depressed patients) may be able to use this as a coping strategy. Unfortunately, depressed patients also show weaker than average connection of brain regions within the Frontoparietal Network [4], or FPN, pictured above in green. This network goes by different names, (Central Executive Network, Executive Attention Network, etc.), but one of its primary roles is as the director of one’s executive attention. In other words, you use it to think about what you want to think about. As a result of decreased efficiency of the FPN, depressed people may experience a decreased ability to control their thoughts. This has been theorized to help explain the high comorbidity rates of ADHD and Depression. The ability to cognitively escape from one’s depressive thoughts or ideas can be particularly difficult to achieve in this case.
Takeaways
So, to summarize, for a depressed person, it is entirely possible that: the bad feels worse, the good doesn’t feel like anything much, you keep thinking of the bad—no you really keep thinking about the bad—you can’t stop. Surely, anyone can imagine this would make someone feel quite dejected, despondent, and maybe even hopeless. The good news, however, is that there are effective treatments for even severe depression. Research shows that in patients who do receive corrective treatment to enhance or diminish a certain connection, typical patterns of connectivity are likely to develop[6]. This means that not only do today’s treatments alleviate symptoms, but due to the brain’s plasticity, may even serve to improve endogenous (i.e. natural, unmedicated) brain function over time—improving the person’s quality of life!
This is by no means a comprehensive scientific explanation of depression—such an explanation is not currently possible. This article does, however, aim to highlight that depression (like any medical ailment), is a physical illness with real, tangible, mechanistic causes—and that those causes can be addressed. Depressed people should be encouraged to seek medical care.
~ Gabe Sweezy

Gabe Sweezy is an undergraduate student of neuroscience and a premedical student at Saint Louis University. As a student of cognitive neuroscience with a passion for mental health, Gabe is particularly interested in the biological processes underlying mental illnesses.
This research article is supervised and sponsored by Faculty Sponsor, Dr. Brenda Kirchhoff Ph.D.
References
[1] Cheng W;Rolls ET;Qiu J;Liu W;Tang Y;Huang CC;Wang X;Zhang J;Lin W;Zheng L;Pu J;Tsai SJ;Yang AC;Lin CP;Wang F;Xie P;Feng J; (2016, October 14). Medial reward and lateral non-reward orbitofrontal cortex circuits change in opposite directions in depression. Brain : a journal of neurology. Retrieved February 1, 2022, from https://pubmed.ncbi.nlm.nih.gov/27742666/
[2] Davey CG;Whittle S;Harrison BJ;Simmons JG;Byrne ML;Schwartz OS;Allen NB; (2014, August 27). Functional brain-imaging correlates of negative affectivity and the onset of first-episode depression. Psychological medicine. Retrieved February 1, 2022, from https://pubmed.ncbi.nlm.nih.gov/25162634/
[3] Frazer, A. (1999, January 1). Serotonin receptors. Basic Neurochemistry: Molecular, Cellular and Medical Aspects. 6th edition. Retrieved February 2, 2022, from https://www.ncbi.nlm.nih.gov/books/NBK28234/
[4] Goeleven E;De Raedt R;Baert S;Koster EH; (n.d.). Deficient inhibition of emotional information in depression. Journal of affective disorders. Retrieved February 1, 2022, from https://pubmed.ncbi.nlm.nih.gov/16647141/
[5] Greicius, M. D., Flores, B. H., Menon, V., Glover, G. H., Solvason, H. B., Kenna, H., Reiss, A. L., & Schatzberg, A. F. (2007, September 1). Resting-state functional connectivity in major depression: Abnormally increased contributions from subgenual cingulate cortex and thalamus. Biological psychiatry. Retrieved February 1, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2001244/
[6] Li, B.-J., Friston, K., Mody, M., Wang, H.-N., Lu, H.-B., & Hu, D.-W. (2018, November). A brain network model for depression: From symptom understanding to disease intervention. CNS neuroscience & therapeutics. Retrieved February 1, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6490158/
[7] Pandya, M., Altinay, M., Malone, D. A., & Anand, A. (2012, December). Where in the brain is depression? Current psychiatry reports. Retrieved February 1, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3619732/

